Nonsurgical Root Canal
Frequently Asked QuestionsWhat is non-surgical endodontic treatment?
This is a method of treating the inside of the tooth, also known as a root canal treatment. It is one of the most common dental procedures that can be performed to prevent tooth loss.
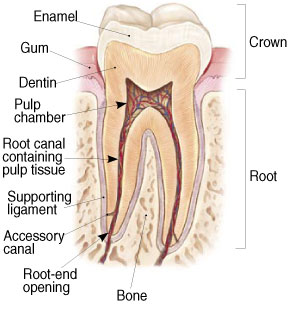
The pulp can be found in the center of the tooth and can extend all the way to the tip of the roots where it connects to the tissues surrounding the root. The pulp has a very important role during a tooth’s development. However, a tooth that has reached full maturity can survive without the pulp, because it continues to receive nourishment by the surrounding tissues.
Why do I need endodontic treatment?
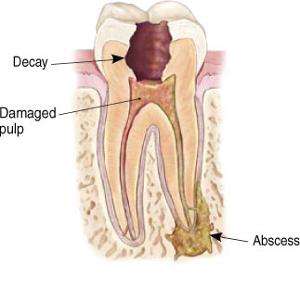
If the soft tissue inside the root canal of a tooth becomes inflamed or infected, then a root canal treatment is necessary. There can be a variety of factors that cause the inflammation or infection such as: repeated dental procedures on the tooth, deep decay, cracks or chips in the tooth.
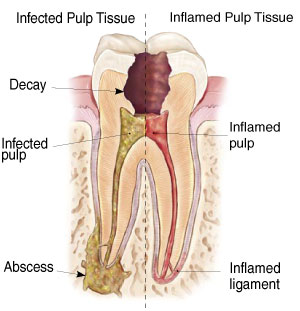
Indication signs to look for include pain, tenderness to touch and chewing, prolonged sensitivity to hot or cold, discoloration of the tooth, swelling of the surrounding tissue, and drainage. Symptoms may not always be present.
How does endodontic treatment save the tooth?
The endodontist removes the inflamed or infected pulp, carefully cleans and shapes the inside of the canal, a channel inside the root, then fills and seals the space. Afterwards, you will return to your dentist, who will place a crown or other restoration on the tooth to protect and restore it to full functions. After restoration, the tooth continues to function like any other tooth.
Endodontic Procedure
Endodontic treatment can often be performed in one or two visits and involves the following steps:
The endodontist examines and x-rays the tooth, then administers local anesthetic. After the tooth is numb, the endodontist places a small protective sheet called a “dental dam” over the area to isolate the tooth and keep it clean and free of saliva during the procedure.
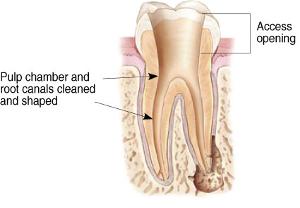
The endodontist makes an opening in the crown of the tooth. Very small instruments are used to clean the pulp from the pulp chamber and root canals and to shape the space for filling.
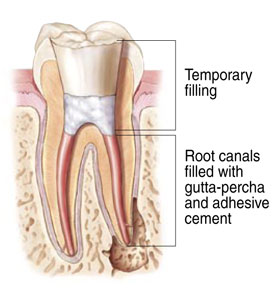
After the space is cleaned and disinfected, the endodontist fills the root canals with a biocompatible material, usually a rubber-like material called “gutta-percha.” The gutta-percha is placed with an adhesive cement to ensure complete sealing of the root canals.
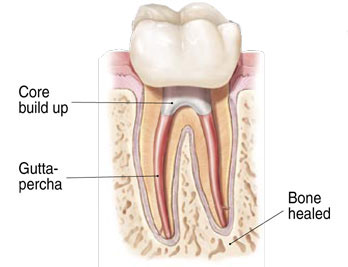
After the final visit with your endodontist, you must return to your dentist to have a crown or other restoration placed on the tooth to protect and restore it to full function.
Will the tooth need any special care or additional treatment after endodontic treatment?
The unrestored tooth is susceptible to fracture, so you should see your dentist for a full restoration as soon as possible. Otherwise, you need only practice good oral hygiene, including brushing, flossing, and regular checkups and cleanings.
Most endodontically treated teeth last as long as other natural teeth. In rare cases a tooth that has undergone endodontic treatment does not heal or the pain continues. Occasionally, the tooth may become painful or diseased months or even years after successful treatment. Often when this occurs, redoing the endodontic procedure can save the tooth.
What causes an endodontically treated tooth to need additional treatment?
New trauma, deep decay, or a loose, cracked or broken filling can cause new infection in your tooth. In some cases, the endodontist may discover additional very narrow or curved canals that could not be treated during the initial procedure.
Can all teeth be treated endodontically?
Most teeth can be treated. Occasionally, a tooth can’t be saved because the root canals are not accessible, the root is severely fractured, the tooth doesn’t have adequate bone support, or the tooth cannot be restored. However, advances in endodontics are making it possible to save teeth that even a few years ago would have been lost. When endodontic treatment is not effective, endodontic surgery may be able to save the tooth.
Focal Infection Theory – Are root canals making me sick?
The focal infection theory, first articulated and popularized in the early 1900s by figures in the medical community such as EC Rosenow and William Hunter, attempted to draw a direct connection between infected or endodonticaly treated pulpless teeth with numerous maladies of the day including pale complexion, chronic dyspepsia, anemias, intestinal disorders, and nervous complaints. Dr. Weston Price, an American dentist and researcher, conducted extensive studies in the field of endodontics in the early 20th century which appeared to support the theory. Careful review of his publications show significant flaws in his study design, techniques, methodology, and case follow up which cause his conclusions to be highly suspect. His research did inspire future work in bacteriology, immunology, and the safety and efficacy of root canal treatment.
The later research inspired by Dr. Price’s findings laid the foundation for modern root canal therapy and rationale underlying it. Adequately designed research studies performed in the 1930s provided evidence to refute the focal infection theory. Substantial work done since the 1930s has consistently provided evidence that the focal infection theory is not valid. Dr. Price’s results have never been successfully replicated. In 1993, Dr. George Meinig with his book Root Canal Cover-up Exposed! Many Illnesses Result, brought the focal infection theory back to public attention. In the book, Dr. Meinig presents Dr. Price’s findings and conclusions and uses them as a basis on which to recommend that concerned patients consider having their root canal treated teeth extracted. Dr. Meinig also asserts that the findings of Dr. Price had been suppressed by self-interested dentists. Dr. George Meinig is a founding member of the American Association Endodontists. All current good evidence suggests that root canal treatment does not cause systemic disease as suggested by the focal infection theory. We would not be providing this treatment if it did.
Will I feel pain during or after the procedure?
Many endodontic procedures are performed to relieve the pain of toothaches caused by pulp inflammation or infection. With modern techniques and anesthetics, most patients report that they are comfortable during the procedure. For the first few days after treatment, your tooth may feel sensitive, especially if there was pain or infection before the procedure. This discomfort can be relieved with over-the-counter or prescription medications. Follow your endodontic's instructions carefully. Your tooth may continue to feel slightly different from your teeth for some time after your endodontic treatment is completed. However, if you have severe pain or pressure or pain that lasts more than a few days, call your endodontist.
How much will the procedure cost?
The cost varies depending on how complex the problem is and which tooth is affected. Molars are more difficult to treat and therefore are usually more. Most dental insurance policies provide some coverage for endodontic treatment.
Generally, endodontic treatment and restoration of the natural tooth are less expensive than the alternative of having the tooth extracted. An extracted tooth must be replaced with a bridge or implant to restore chewing function and prevent adjacent teeth from shifting. These procedures tend to cost more than endodontic treatment and appropriate restoration. With root canal treatment you save your natural teeth and money.
